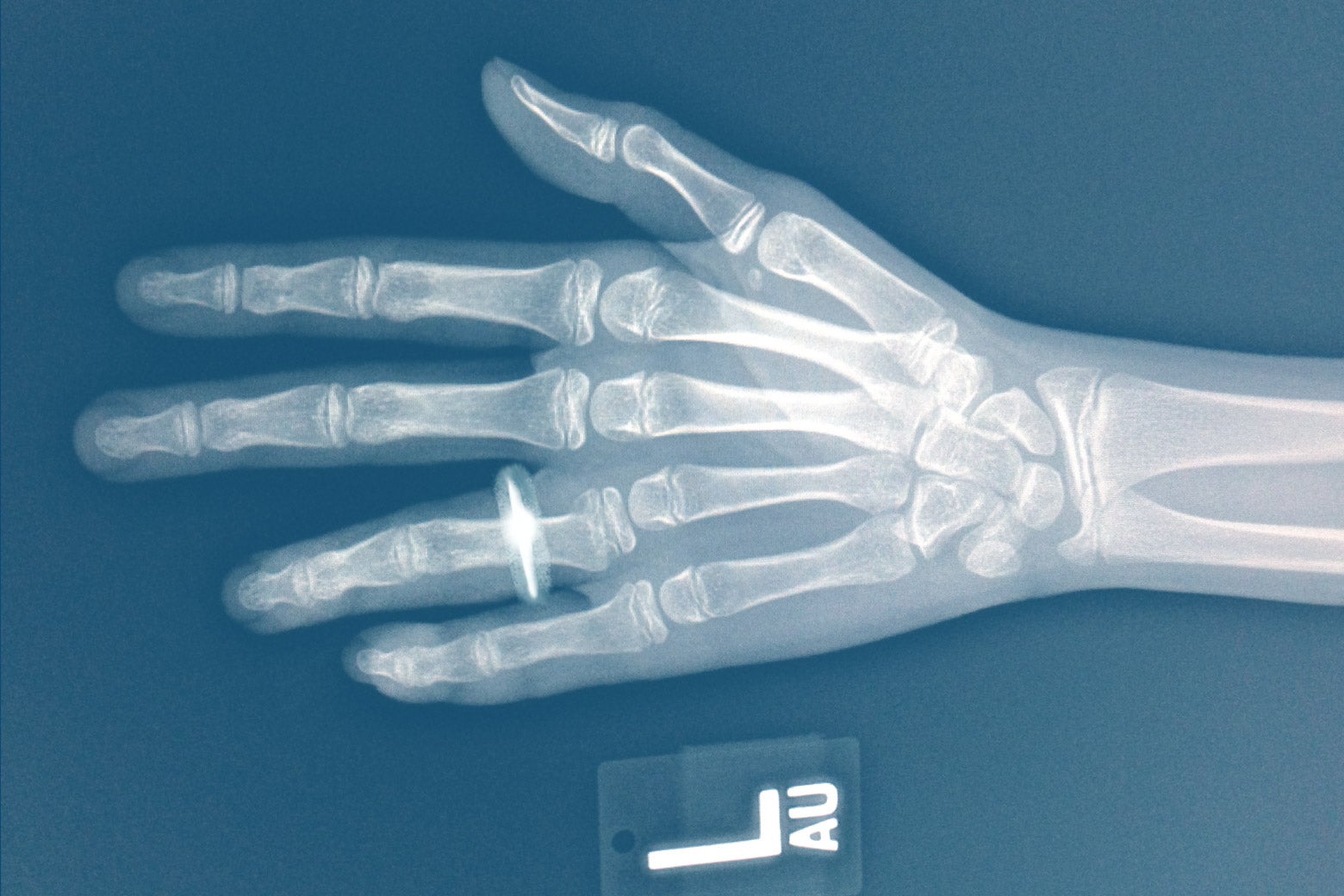
“I know those bones!” I thought to myself, looking at a tweet. It was an X-ray of the broken hand of a patient whom I had treated in my emergency department a few weeks prior. The image had no identifying information that would violate anyone’s privacy, but it was a remarkable and strange feeling to recognize a person by an X-ray. But what shook me was the commentary that accompanied the image: It said the pattern of this particular fracture was highly suspicious for intimate partner violence. I had not remotely considered that possibility when treating the patient. It had been what we physicians call “a good story”—meaning that it was credible, and that my physical findings matched the description of what the patient said had caused it (an item falling). I didn’t suspect a thing.
What, I wanted to know, had made this X-ray look suspicious to my colleague, emergency radiologist Dr. Bharti Khurana, who had posted the tweet? Answers to questions like this are just starting to emerge: This month, Khurana and her colleagues here at Brigham and Women’s Hospital in Boston published what may turn out to be a game-changing study describing the radiographic findings in intimate partner violence in the journal Radiology. The study gives front-line physicians like me powerful information about both the demographics and the patterns of injury seen in domestic violence. We already know that unusual patterns of broken bones help doctors detect child abuse. This new study suggests that such an approach may be successful in adults too.
Some of her team’s findings confirm what we might have suspected, but others are surprises. For example, it’s widely understood that injuries to the head and face are the strongest indicators of domestic violence, particularly because there are few other causes of such injuries. But Khurana and her colleagues also found that injuries to the arms and legs may present good opportunities for detection. These kinds of fractures are actually more common in domestic violence victims than facial or head injury; the problem is that they’re more common in everyone else, too. What Khurana and her colleagues are now trying to assess and quantify are what types of arm and leg fractures are more commonly associated with domestic violence, to give doctors a clearer sense of what type of break to look for.
It doesn’t take tremendous medical judgment to be concerned if a woman has a broken nose and a black eye, but who gets suspicious about a fracture to the fifth metacarpal bone? And yet, as Khurana explains, the type of injury in my patient was indicative of a “defensive” injury to the long bone of the hand. While attackers (and also boxers) tend to break the long bone nearer to the fingers, defensive injuries to that same bone are often closer to the wrist.
They could also simply be the result of an unusual break or, in the case of my patient, an object falling and landing weirdly. So how should doctors act on this knowledge, particularly given that we currently lack data that would help us understand how statistically valid such observations are? Here doctors have to tread carefully.
The deeper issue, according to Brigham and Women’s Hospital emergency physician Dr.
Hanni Stoklosa, who co-authored the paper and studies intimate partner violence and human trafficking, is how hard it is to detect intimate partner violence. “Medical screening is easy. You ask a question, you get an answer,” she says. But domestic violence survivors tend to underreport to health care providers. This is often multifactorial, but one barrier might be that health care providers in many states are required to notify law enforcement authorities about domestic violence. As my friend Daryl E. Bassin, a former deputy city attorney for Anaheim, California, has often recounted, survivors can have legitimate fears about involving law enforcement, including that incarceration or in some cases deportation of an accused perpetrator would deprive a family of financial or food security. “Our job is to create the right conditions for disclosure, and, if and when they are ready, we let them know that this is a safe place to go,” Stoklosa says.
This is why my protocol when I suspect intimate partner violence has changed over time. Interviewing a patient alone is often crucial. Survivors frequently come to the emergency department with their abusers, and it is not until they are alone that they feel safe saying what really happened. I also remind patients that my job is to take care of them and that I do not work for the government or for law enforcement. I am legally obligated to report intimate partner violence in certain specific cases; in Massachusetts, where I practice, the threshold is if a firearm, knife, or similar weapon was used, or if the patient has burns covering more than 5 percent of the body. Each state has different requirements.
Radiologists literally have X-ray vision, and the clarity of that vision appears to be improving. Emergency physicians should know that we already have resources in place for survivors of intimate partner violence—and we can probably use them more often. That might mean calling a social worker directly into the emergency department to help survivors find safe housing, make a police report (if that is what they want), and provide resources and numbers to call if and when they want more help in the future. We can also hope that continued analysis will keep giving us better indicators of when to act. For me, this new research was a useful reminder of how important it always is to consider the whole patient, rather than just the injured body part.
The opinions expressed in this article are solely those of the author and do not reflect the views and opinions of Brigham and Women’s Hospital.